What is an infection?
Causes of infection, otherwise known as pathogens, include viruses, bacteria and fungi. Infection happens when pathogens enter the body and begin to multiply, making you unwell. Infections can cause a variety of symptoms depending on where they are located. General symptoms of infection include fever, chills, pain, fatigue and feeling generally unwell. Infections are usually treated with medications called antimicrobial medications. Antibiotics, which fight bacteria, are a common example. Serious infections may require treatment in hospital.
Why is reducing infection risk important in patients with myeloma?
Infection is a leading cause of illness for myeloma patients, and it can be life-hreatening. It is therefore important to consider preventative measures to reduce the risk of infection. These preventative measures can form part of an individualised treatment plan that is adapted to the level of risk. Infection risk is elevated in all stages of myeloma due to myeloma itself, myeloma medications and patient factors such as age and other illnesses (also called comorbidities). In the first year after diagnosis, myeloma patients are seven times more likely to experience infection than people without myeloma, and of the myeloma patients who die within one year of diagnosis, 27% of deaths are related to infection. You can read more about infection risk associated with myeloma and myeloma treatments in the Q&A Infection risk with myeloma and myeloma treatments.
Medications that use the patient’s immune system to work such as bispecific antibody medications and CAR T-cell therapies present higher risks of infection than other medications, which can persist in the long-term.
What medications aim to reduce the risk of infection in myeloma?
Several medications can potentially reduce an individual’s risk of infection when they have myeloma. They are each used under specific and personalised circumstances.
These medications include:
- Prophylactic (i.e., preventative) antimicrobial medications. Antimicrobial medications, such as antibiotics, taken regularly to prevent infection before it occurs.
- Granulocyte Colony Stimulating Factor (GCSF) e.g. filgrastim. Medication to stimulate production of neutrophils (a type of white blood cell) that fight infection. This can treat neutropenia, which is when neutrophil levels are low.
- Vaccines. Medications designed to train the immune system to recognise a specific virus or bacteria (pathogen) and prevent infection from developing when the body is next exposed to that pathogen.
- Immunoglobulin replacement therapies. Immunoglobulins are proteins made by the body in different shapes that stick to different pathogens which kills them. Myeloma medications can cause the proteins to become low, so they can be replaced by immunoglobulin medications derived from human plasma donations.
What are prophylactic antimicrobial medications?
Prophylactic antimicrobials are taken to prevent infection. Antimicrobials are medications that kill infection-causing pathogens such as bacteria, viruses and fungus. They are generally taken orally and include the following:
- Antibiotic medications to prevent against bacterial infections e.g. levofloxacin
- Antiviral medications to prevent against viral infections e.g. aciclovir
- Antifungal medications to prevent against fungal infections e.g. fluconazole
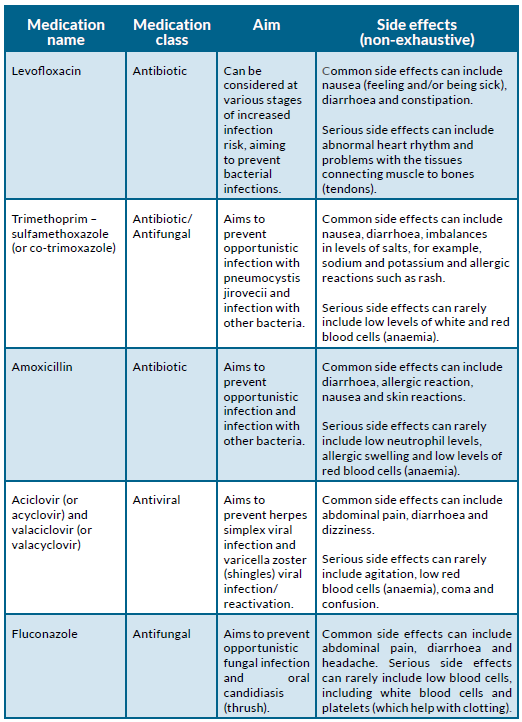
Other common antimicrobial medications prescribed to prevent infections are summarised in the table below. Like most medications, they have side effects. The benefit of taking these medications needs to be higher than the risk of harm from side effects, which is decided by the prescriber (your doctor or nurse). The aim is to prevent infections. These include respiratory tract infections, of which pneumonia (an infection of the lungs) is an example. A common pneumonia type is pneumococcal pneumonia, for which preventative (or prophylactic) amoxicillin is frequently prescribed. Other infections that prophylactic antimicrobials aim to prevent, include urinary tract infections (bladder or kidney infection), sinusitis (infection of the sinuses) and sepsis.
Sepsis is a treatable, but life-threatening condition. Sepsis can occur when infection-causing pathogens are present in the blood and cause a body-wide response. It can cause symptoms such as fever, chills, feeling generally unwell, dizziness, shortness of breath, fast heart rate and decreased urination. Sepsis is an emergency that is usually managed in hospital. Treatment for sepsis includes antibiotics and fluids into the vein (intravenously).
Antimicrobial prophylaxis (preventative medications) can also be prescribed with the aim of preventing opportunistic infections. Opportunistic infection means infection caused by a pathogen that under normal circumstances, when immunity is good, would not cause infection. An example relevant to myeloma patients is a lung infection caused by a fungus called pneumocystis jirovecii.
One risk factor for pneumocystis infection is taking corticosteroid (steroid) medication, such as dexamethasone, which is frequently used to help treat myeloma.
Common prophylactic antimicrobial medications
Prophylactic antimicrobials are taken to prevent infection. Antimicrobials are medications that kill infection-causing pathogens such as bacteria, viruses and fungus. They are generally taken orally and include the following:
- Antibiotic medications to prevent against bacterial infections e.g. levofloxacin
- Antiviral medications to prevent against viral infections e.g. aciclovir
- Antifungal medications to prevent against fungal infections e.g. fluconazole
Other common antimicrobial medications prescribed to prevent infections are summarised in the table below. Like most medications, they have side effects. The benefit of taking these medications needs to be higher than the risk of harm from side effects, which is decided by the prescriber (your doctor or nurse). The aim is to prevent infections. These include respiratory tract infections, of which pneumonia (an infection of the lungs) is an example. A common pneumonia type is pneumococcal pneumonia, for which preventative (or prophylactic) amoxicillin is frequently prescribed. Other infections that prophylactic antimicrobials aim to prevent, include urinary tract infections (bladder or kidney infection), sinusitis (infection of the sinuses) and sepsis.
Sepsis is a treatable, but life-threatening condition. Sepsis can occur when infection-causing pathogens are present in the blood and cause a body-wide response. It can cause symptoms such as fever, chills, feeling generally unwell, dizziness, shortness of breath, fast heart rate and decreased urination. Sepsis is an emergency that is usually managed in hospital. Treatment for sepsis includes antibiotics and fluids into the vein (intravenously).
Antimicrobial prophylaxis (preventative medications) can also be prescribed with the aim of preventing opportunistic infections. Opportunistic infection means infection caused by a pathogen that under normal circumstances, when immunity is good, would not cause infection. An example relevant to myeloma patients is a lung infection caused by a fungus called pneumocystis jirovecii.
One risk factor for pneumocystis infection is taking corticosteroid (steroid) medication, such as dexamethasone, which is frequently used to help treat myeloma.
When and how are prophylactic antimicrobial medications prescribed?
The decision to prescribe prophylactic antimicrobials, and which antimicrobials are prescribed and when, depends on multiple factors. These include:
- The level of infection risk
- The types of myeloma medications the patient is taking (especially whether they are prescribed steroids)
- Whether the benefit outweighs the risk of side effects from the antimicrobial medication
- Patient factors (if kidney function is lower, the dose may be decreased)
- The area the patient lives in and risk of antimicrobial resistance
The level of infection risk
Prophylactic (preventative) antimicrobial medications are more likely to be recommended if the risk of infection is higher. The level of infection risk varies based on other medications given to treat myeloma, level of immunosuppression (how low the immune system function is) from myeloma, and patient factors such as age and other illness. Infection risk is generally highest when newly diagnosed and up to three months after diagnosis, and when treating relapsed/refractory myeloma. The infection risk is also higher if a patient has low white cells in conditions called lymphopenia (low lymphocyte white blood cells) or neutropenia (low neutrophil white blood cells).
Types of myeloma medications
The types of myeloma medications a patient is receiving is an important consideration for antimicrobial prescription. For example, the antiviral medication, aciclovir, is important whilst taking bortezomib (a proteosome
inhibitor treatment), due to bortezomib being associated with developing shingles, which causes a painful rash and can cause further complications.
Shingles is caused by a virus called varicella zoster, otherwise known as chicken pox virus, which can reactivate when people are immunosuppressed if they have ever had chicken pox. Another example is the use of trimethoprim–sulfamethoxazole, an anti-fungal medication, which is beneficial when being treated with steroids long-term (such as cortisone or dexamethasone).
Benefit vs risk
The benefit of taking preventative antimicrobials must be judged to be greater than the risk of the side effects. For example, an antibiotics class called fluoroquinolones, of which levofloxacin is an example, present a risk of rupturing the main tendon (Achilles tendon) of the ankle, amongst other side effects.
Patient factors
Patients may require different prescriptions to account for lower kidney function, as many medications are filtered out of the body by the kidneys. Myeloma can damage the kidneys. It can do this by causing high calcium levels through bone damage, and by producing paraprotein, which is the protein made by the myeloma cells, which can damage the kidneys. Patients may also need alterations based on their weight.
Antibiotic resistance
The country and area where the patient lives are important for antimicrobial choice due to pathogens being able to develop resistance. Pathogens do this by adapting to their environment to survive. Therefore, pathogens in different countries and specific areas are resistant to different antimicrobials or have what is called ‘different patterns of resistance’. Local guidelines are developed by experts in pathogens (such as microbiologists) to help guide prescribers on which antimicrobials will be most effective in that area. The risk of antibiotic resistance developing will be considered by prescribers, because antibiotic resistant infections are more difficult to treat.
If you or someone you care for has been prescribed prophylactic (preventative) antimicrobial medication, and you are unsure of the reason, ask the prescriber to explain this to you (your doctor or nurse). It is important to only take antimicrobials that have been prescribed to you, because of the risks, which include developing antimicrobial resistance.
What is granulocyte colony stimulating factor?
Granulocyte Colony Stimulating Factor (GCSF) is a type of medication taken to stimulate production of neutrophils (white blood cells) that fight infection.
GCSF is generally taken as an injection underneath the skin (usually daily but always check with your prescriber) during periods of neutropenia (low neutrophil levels), until the level has recovered. This is usually monitored through regular blood tests. It can also be given by injection into a vein (intravenously). The recovery time of neutrophil levels can vary, but generally it takes a few days to a week to work. Sometimes it is taken for longer periods. Filgrastim is an example of a GCSF medication. Common side effects include joint pains, inflammation of the blood vessels under the skin and shortness of breath.
What are vaccines?
Vaccines are medications designed to train the immune system to recognise a specific virus or bacteria (pathogen).
Vaccines aim to prevent infections developing by exposing the body to a safe amount of the pathogen, inactive parts of the pathogen, or products of the pathogen called toxins. During vaccination, the body is exposed to antigens, which are proteins specific to that pathogen. The immune system forms a memory of the antigen, so that the next time exposure occurs, the pathogen is removed from the body before infection happens. The body recognises and responds to vaccination by producing specific antibodies (a type of immune protein) to the pathogen.
There are different types of vaccines. Vaccines can be live, or non-live. Non-live vaccines do not contain living pathogens (such as bacteria or viruses) and are recommended for myeloma patients. The different types of non-live vaccines include:
- Inactivated vaccines, which contain dead, whole pathogens
- Subunit vaccines made from a part of a pathogen
- Toxoid vaccines, which contain inactivated toxins produced by the pathogen
- DNA viral vector or mRNA vaccines, which contain instructions for the body
on how to make the harmless parts of the pathogen
In contrast, live vaccines contain living pathogens (such as bacteria or viruses) that have been weakened (attenuated).
It is recommended that myeloma patients avoid live vaccines. This is because there is a risk that live vaccines can cause infection in immunocompromised individuals, such as myeloma patients. In circumstances of well-controlled remission where the immune system of the patient is more effective, and it is recommended by their health-care provider (usually by their haematologist), there may be exceptions to this.
Close contacts of myeloma patients (e.g. family members and carers) are recommended to protect themselves against infection by receiving all age and exposure-appropriate vaccines, to prevent the spread of infection to patients. Where possible, non-live vaccines, instead of live vaccines, are recommended for close contacts of myeloma patients. This is because there is a small risk that live vaccines can cause high enough levels of pathogen to pass on an infection to the myeloma patient. Close contacts can ask the person giving the vaccine whether it is a live vaccine.
Examples of common live vaccines are:
- The nasal spray version of the flu (influenza) vaccine
- MMR (measles, mumps and rubella) vaccine
- Bacillus Calmette–Guérin (BCG) vaccine (tuberculosis)
- Typhoid vaccine (oral route) (note that there are also inactivated typhoid vaccines given by injection)
- Rubella vaccine (German measles)
- Yellow fever vaccine
- Zoster vaccine for shingles (note that there are also inactivated shingles vaccines)
- Chicken pox vaccine (varicella)
Are vaccines effective in myeloma patients?
Vaccination is recommended for myeloma patients to help protect against infection. Often, vaccines are less effective in myeloma patients than in people with healthy immune systems. This is because the immune system is required to respond to make antibodies (proteins of a specific shape that cause the pathogen to be killed) when a vaccine is administered. Myeloma and myeloma medications affect the immune system, so fewer antibodies may be produced. This is because myeloma is a cancer of plasma cells, which are cells that normally produce antibodies. Myeloma patients can still produce antibodies with their healthy plasma cells, but the myeloma cells (cancerous plasma cells) affect the healthy plasma cells’ ability to do this.
However, vaccinations are still recommended for myeloma patients.
What vaccinations should myeloma patients receive?
Patients should follow advice from their treating haematologist on which vaccines to receive and when.
They can give advice on when vaccination is recommended and may facilitate the most effective response depending on the myeloma treatment schedule.
Vaccinations that are commonly recommended to myeloma patients include (non-exhaustive list):
- Inactivated influenza vaccine – to protect against flu, usually recommended annually
- Covid-19 vaccines – vaccination and boosters (repeated vaccinations to top up immunity and protect against new covid variants) are recommended for myeloma patients
- Inactivated pneumococcal vaccine – to protect against lung infection caused by pneumococcal bacteria
- Recombinant zoster vaccine – to protect against shingles (reactivation of the chicken pox virus)
Vaccination may be recommended more than once for the same pathogen, such as pneumococcal vaccination, to increase protection. Seasonal vaccines like influenza and Covid-19 change annually depending on which variants of the virus are most prevalent. Therefore, it is necessary to consider regular, seasonal vaccination.
Other vaccinations of note include vaccination against haemophilus influenzae, which is a bacterium that can cause nose and throat infection as well as meningitis (inflammation of the tissue around the spinal cord) and sepsis. Vaccination against this can be considered in myeloma patients. Hepatitis B virus vaccination may be recommended for patients at particular risk (for example, living in areas where levels of the virus are high). Vaccination against meningococcal bacteria may also be recommended to prevent bacterial meningitis.
Patients who undergo a stem cell transplant with high dose chemotherapy may no longer be immune to diseases they were vaccinated against as a child. This is because the immune system loses its memory of these pathogens due to the high doses of chemotherapy. To reacquire immunity, these patients may be offered a schedule of vaccinations 6-12 months after their stem cell transplant that include common childhood vaccinations such as an inactivated polio vaccine and tetanus vaccine.
Patients treated with CAR T-cell therapies (a type of immunotherapy which uses the patient’s immune system to target the myeloma cells) may also need vaccination with common childhood vaccines following treatment. However, further data from clinical trials is required to study the extent to which childhood vaccination immunity is lost and how effective vaccination is in patients treated with CAR T-cell therapies.
What are immunoglobulin replacement therapies?
Immunoglobulins are proteins made by the body in different shapes that recognise different pathogens and cause them to be killed by other immune cells.
Myeloma treatments can cause immunoglobulins to become low. This condition is called secondary hypogammaglobulinemia (secondary because it is caused by a disease, in this case, myeloma).
Immunoglobulin replacement therapies can be used to treat this condition. It is made from many different donations of human plasma (the clear coloured part of the blood, without blood cells). The immunoglobulins are extracted and concentrated into a liquid medication that can be given by injection into the vein (intravenously, IV), or under the skin (subcutaneously, SC).
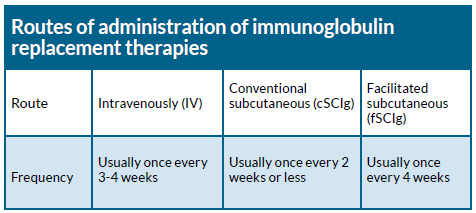
Intravenous immunoglobulin (IVIg) replacement therapy is usually given once every three to four weeks whilst the treatment is needed. This will mean the patient needs intravenous access, for example, via a temporary intravenous cannula using a needle to place a plastic tube into the vein for the duration of the infusion. The setting for this treatment is usually a hospital, outpatient clinic, or at home.
There are conventional subcutaneous (through the skin) immunoglobulin replacement therapies (cSCIg) and facilitated subcutaneous immunoglobulin replacement therapies (fSCIg). Both can be self-administered at home. Patients or their carers can be taught to administer the medication. For cSCIg, the injections are every two weeks or more frequently. fSCIg can be given less frequently, up to every four weeks, because it allows for bigger doses to be administered.
Side effects of immunoglobulin replacement therapies vary depending on the route of administration. IV administration commonly causes headaches, migraines, fatigue, chills, dizziness, nausea and vomiting. These also occur with SC administration, but less frequently. SC administration is more commonly associated with localised injection site reactions such as itching, which is infrequent with IV administration. Both SC and IV can cause more serious side effects such as severe allergic reactions. This is not an exhaustive list, and it is recommended to always discuss side effects with your doctor or nurse.
Which myeloma patients receive immunoglobulin replacement therapy?
Immunoglobulin replacement is not routinely recommended in all circumstances. For example, in clinical trials no significant reduction in infection rate was found to occur from using immunoglobulin replacement during autologous stem cell transplantation (ASCT). In 2022, the International Myeloma Working Group recommended that the use of immunoglobulin medications be reserved for when immunoglobulin levels are below a threshold of 400mg/dl in patients who have severe and recurrent infections, despite vaccinations and prophylactic antimicrobial medications, or for patients who have life-threatening infections.
Practices may vary across Europe.
Hypogammaglobulinemia can occur after treatment with medications that use the patient’s immune system to work, such as bispecific monoclonal antibody medications and CAR T-cell therapies, which has highlighted the importance of research into the effects of immunoglobulin replacement therapies in these circumstances. Whilst patients are taking bispecific monoclonal antibody medications, the current recommendation from an expert panel in 2023 is to start immunoglobulin replacement monthly if immunoglobulin levels are below the threshold of 400mg/dl, and to continue while the levels remain low, even if there are no infections. Similarly, prophylactic (preventative) immunoglobulin replacement can be considered after CAR T-cell therapies if immunoglobulin levels are below the threshold of 400mg/dl, initially in the absence of infections.
Once again, practices may vary across Europe and access to immunoglobulin replacement therapies also varies.
What general actions can be taken to reduce infection risk for myeloma patients?
Other strategies that can be taken to reduce infection risk include:
- Regular handwashing to help the reduce risk of spreading pathogens that cause infection.
Handwashing can help reduce infections that are spread through direct contact, such as cold and flu viruses. Patients may also wear a facial mask if recommended. - Personalised advice to patients and carers can be given from healthcare professionals (i.e. your doctor or nurse) on infection prevention and risk. Personalised advice can help patients and carers feel empowered. Infection risk varies depending on the stage of treatment and many other factors. This can be communicated by healthcare providers to patients and carers. This facilitates confident decision making on how to manage protecting themselves against infection whilst maintaining a good quality of life. It can also help patients and carers understand why certain medications and vaccines are being recommended. It is important for good mental health and quality of life to be able to engage in family life, such as caring for children or grandchildren. Patients should seek individualised advice from their doctor or nurse on practical steps they can take to balance managing risk of infection with spending time with friends and family.
- Avoiding crowded places and situations where contracting infection is more likely.
This may be necessary, especially at times when infection risk is higher. Where there are more people present, there is a higher likelihood of one person having an infection that can spread through touch, water droplets, or through the air. This may mean travelling on public transport during more quiet times, and when spending time with family and friends, you can inform them of your higher risk of infection so that precautions can be taken, such as delaying visits if they are unwell and could pass on infection. - Seeking specialist travel advice if this is available, as extra vaccines may be recommended. When patients travel, the risk of different infections that are more common in the country of interest should be considered. Therefore, patients should seek personalised advice when looking to travel, as there may be extra vaccinations available to help reduce the risk of infection.
- Being tested for viruses such as hepatitis B, hepatitis C and HIV before starting myeloma treatment.
This can alert patients and clinicians to the risk of an existing virus getting worse after immunosuppressive treatment. - Making alterations to food preparation and diet whilst patients are neutropenic.
In general, no specific diet is recommended to patients with myeloma, though it is important to emphasise that a healthy, balanced diet can help to support immune system function. Whilst patients have low levels of neutrophils (a type of white blood cell), which is called neutropenia, it is recommended that they follow specific advice. Bacteria and other microorganisms found in food can cause serious infection whilst patients are neutropenic, which would not develop if neutrophil levels are within the normal range. Dietary advice for patients who are neutropenic in general aims to help them reduce the risk that food becomes contaminated with bacteria and avoid foods that naturally contain pathogens, such as raw meats and fish, or unpasteurised dairy products.
Food preparation and storage advice whilst neutropenic
- Refrigerate or freeze fresh food immediately after buying
- When defrosting food, do not defrost by leaving food out on the counter, and cook defrosted food immediately
- Ensure hands are clean when handling food
- Use separate cutting boards for meat, fish and other produce, and avoid wooden cutting boards
- Clean dishes with soap and water that have held raw meat or fish before using again
Foods to avoid whilst neutropenic
Whilst neutropenic, it is important that patients avoid foods that have pathogens such as bacteria in them. These include:
- Dairy: unpasteurised milk or cream, for example, some soft-serve ice creams, soft cheeses that are mould-ripened (have a soft white coating on the outside) such as brie, soft blue cheeses, probiotic drinks or yoghurts
- Eggs: raw or runny eggs or food containing raw eggs
- Fruit and vegetables: damaged or bruised fruit and vegetables or uncooked sprouted seeds
- Fish and seafood: smoked fish, such as smoked trout or salmon, raw fish or raw shellfish
- Meat and poultry: raw and undercooked meat and poultry, unpasteurised pâté, cured or smoked meats
- Loose foods: black pepper, dried herbs and spices bought loose and any foods from places where people serve themselves, due to the risk of contamination by other people
Summary
- Infections are common in patients with myeloma and can be life-threatening
- Infection prevention is important for myeloma patients and strategies can be based on an individual’s risk, which may change over time
- Regular handwashing is fundamental and wearing a facial mask when needed is recommended
- Medications that work by using the immune system (bispecific monoclonal antibody medications and CAR T-cell therapies) are associated with high risk of infection
- Medications can be used to reduce the risk of infection occurring. These include preventative (prophylactic) antimicrobial medications, Granulocyte Colony Stimulating Factor (GCSF e.g. filgrastim), vaccination and immunoglobulin replacement therapies.
- Myeloma patients are recommended to be vaccinated against flu (influenza), Covid-19, pneumococcus (a type of bacteria that can cause lung infection) and shingles
- Myeloma patients should avoid live vaccines unless informed otherwise
- Patient carers and healthcare professionals are recommended to seek appropriate vaccinations
- General strategies can be taken to reduce infection risk such as seeking travel advice, avoiding crowded places and following food preparation and storage guidelines
- Healthcare professionals can help patients and carers to stay educated their infection risk to aid informed decision making about preventative medications and lifestyle precautions